Some emergencies make a dramatic appearance and leave no doubt as to the diagnosis. Others, like methemoglobinemia, creep in quietly, disguised as “maybe she’s just a little cold.” This rare condition turned an otherwise routine dental appointment into a life threatening scenario for Dr. Zack Flint and his team—and gave us all a chance to refresh our understanding of an often-overlooked complication. The following is from an interview with Dr. Flint who has honorably agreed to share his experience with everyone so if any of us were to encounter this situation, we may be even more prepared. After his recount of the situation, there are some follow up questions he has answered coupled with a few images from the incident. I know this is quite a bit longer than we normally do, but I urge you to take the time to read.
Dr. Zack Flint’s Story
Written by Dr. Flint:
I had a scary situation at my office yesterday that I would like to post about. I'm beating myself up about how I handled a few things and I hope this post might help someone out. I don't care for anonymous posts so I'm going to look like a complete idiot. And that's okay. I apologize for the length but hope that my experience can help someone else make a better call sooner in an emergency situation.
I had an opening in my schedule at the end of the day yesterday. We have an 18-year old that we hired to help out with sterilization and to float assist. Her mom works at the front desk so it was an easy hire. She needed a #15 DB fill so we put her in the schedule. I'll just refer to her as the "patient" from here on out. I placed some benzocaine and administered 1 carp of articaine. Did the filling, but at the end I noticed that her lips were a little blue. I asked her about it and she said she felt fine but hadn't really had any food during the day. Given that she felt fine I assumed it was nothing and left for the day.
I got a call about 10 mins later from my assistant saying that the patient had since turned more blue and was starting to feel different. I had them put her on oxygen and lay her back. I also had them hook up our capnography equipment so that we could get a read on her oxygen saturation. Of course as I'm heading back to the office I get stuck in a bit of after school traffic. So it was taking me a few mins longer to make it back than I would have liked.
I called my assistant again as I was almost back to the office to get an update on the situation. I asked what the O2 saturation was and she told me 73%. My heart immediately started to race and I told them to pack her up to get her to the ER ASAP. This was one mistake I made. I should've told them to call 911. I'm mad at myself for not doing that at this point.
I show up and I look at our staff member and she was BLUE. Our office is situated a few blocks from the ER so I told her mom that we just needed to get here there ASAP. The symptoms were showing up at this point and she had a bad headache and said it was getting harder to hear. She also reported that it felt like her heart was racing a bit. With that being said she was walking perfectly fine. We loaded her up in the car and I told her mom to report what they found out.
I took only a few steps away from the car when I hear her mom start to scream. I look back and see that the patient is slumped over and unconscious in the front seat. I told her mom to call 911 at this point. I sprinted around to the passenger side of the car and when I open the door I noted that the patients chest was no longer moving and I couldn't detect her breathing. Mom is understandably freaking out and I remind her once again to call 911. I unbuckled the patient, lifted her out of the car, and carried her now lifeless body over to some grass right next to the car in front of our office. My assistants noticed me carrying her and asked me what I needed and then sprinted for the AED and crash cart.
When I placed her down in the grass I still couldn't detect any breathing, and it was difficult because I'm still trying to keep her mom calm enough to call 911 while I was assessing the situation. Patient is getting increasingly blue by the second. She was blue from head to toe. Mom was too frazzled and couldn't figure out how to use her phone so I just had to yell out for someone else to call 911.
Right before I'm getting ready to initiate chest compressions I see the patient take a little breath. I then began to pat her on the face again to try and get a response from her. Finally, I get a little flutter of her eyes and they open ever so slightly. My assistants and I began to do some assisted breathing with the ambu bag, and little by little the patient started taking bigger breaths, albeit very labored. Another assistant was getting the AED out and set up. The patient started to get minimally better, but was still getting more blue. But I was just happy to see some progress.
To my relief the fire department showed up in decent time and took over. When I took a step back I noticed that all of my team members had tears in their eyes and were shaking. Mom was crying. The emotions of the situation started to hit me and my hands began to shake in all honesty. They just witnessed their friend and daughter essentially die right in front of them.
Talking to the EMTs I told them that I learned about a disease in dental school called Methemoglobinemia but that it's rare couldn't be sure that's what was going on, obviously, but I just hope the information might help. They felt like it could be a pulmonary embolism which seemed reasonable as well.
When they got her to the ER her oxygen saturation was at 63% and dropping. After running some tests they came to the conclusion that it was probably methemoglobinemia and they administered methelyne blue. Her O2 saturation shot back up and her life was saved. She had to spend a night at the ICU but was discharged today.
I look back now and see the mistakes I made. We got very lucky that we didn't lose a loved member of our staff. If mom would've made it out of the parking lot I have no doubt that this girl would've died on the road in traffic with her mom unsure as to what to do. And thank God the patient didn't leave the office immediately after her filling and try to drive home. I
should've had them call 911 so much sooner. Probably when they initially called me which would've been about 10-15 mins sooner.
But I'm proud of my team. We had our in-office BLS training about a month ago and it paid off as they did such a great job. It honestly saved this girl’s life yesterday. She lived so it's a success overall. I just recognize that perhaps I could've made some better calls early on that would've made things go more smoothly.
In the end it was the Q-tip with benzocaine that set all this in motion. I'm considering eliminating this step from my protocol even though it's rare that this event could happen. Here's a pic of me visiting her in the ICU. When I saw her she said, "Good thing you were there Dr. Flint. If it would have been just my Mom there I would be dead!" She laughed. Her mom laughed. I laughed. And then I went home and had some nightmares. I'm only 2 years out. I don't want to do this ever again...
Interview Questions
Before this event, what was your level of awareness about methemoglobinemia as a potential complication?
"I had heard of it and had a very vague memory of a powerpoint slide from dental school. Initially, it wasn't at the top of my list of what was going on with the patient. However, it must have been when I noticed how blue the patient was that the faint memory of this disease popped back into my head."
What was the very first sign that something was wrong?
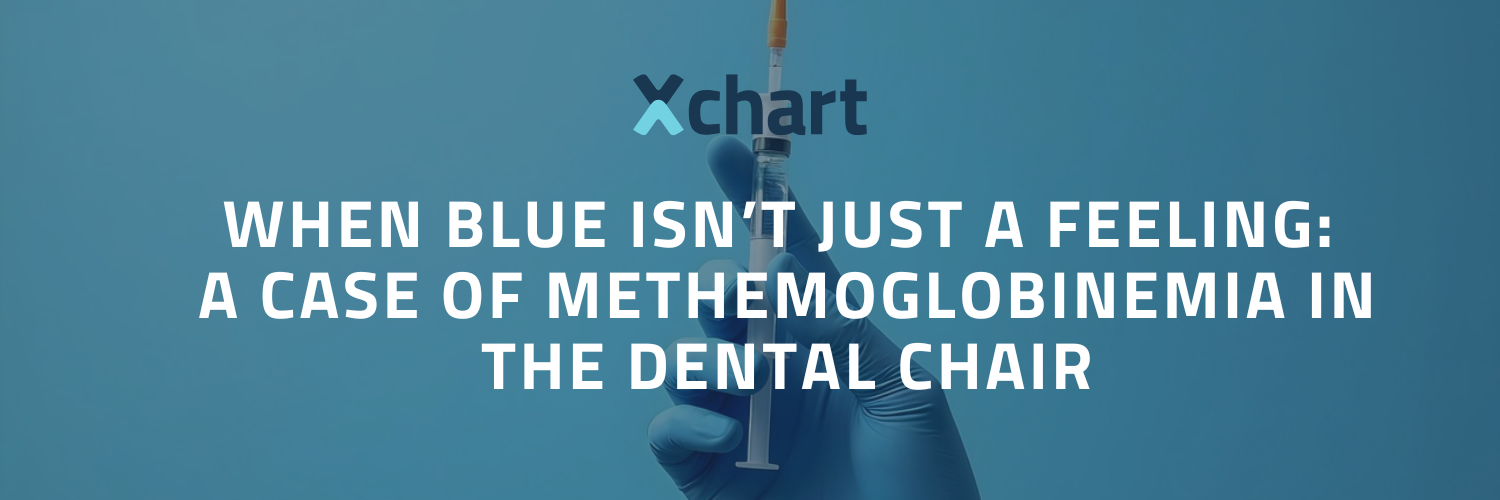
"The patients lips turned slightly blue during the polishing stages of the filling at the end of the appointment. But it was nothing that seemed at the time to be an emergency and I was able to convince myself of a bunch of other things that it may have been. Including the fact that the patient is very pale and was likely a little cold."
How did the patient present physically? Exactly what type of monitoring were you able to achieve? (capnography, pulse oximetry, ECG, BP)
"Upon returning to my office the patient appeared much more blue. Not necessarily blueberry blue, but head to toe she had a blue hue to her. She wasn't shaking or anything like that, but had a headache and stated that her hearing seemed a bit muffled and her heart was beating faster. We have an [anesthesia monitoring] machine (IM60-GT) which monitors capnography, pulse oximetry, ECG, and BP. BP was a slightly lower than what she presented with. ECG was normal.
In the moment, what was going through your mind? Which possible complications were you considering?
“My mind was racing a bit trying to figure things out. First thing was that we needed to get her to the ER. I was also outwardly trying to appear as calm as possible so as to not incite panic into those around me. I assumed at the time that it had to be a response to the articaine, maybe a response to the epinephrine, that was causing it. I believe that it was at this point, given the patient’s color, that methemoglobinemia popped into my head. However, conditions such as heart conditions (although ECG was normal), pulmonary embolism, and respiratory concerns still had to be considered.”
How did your team respond, and what was the sequence of actions you took in those first few minutes?
“My team which consisted of 2 assistants, a hygienist, and the patient’s mom who is one of our front desk staff members. The team was very responsive to all of my instructions. When I told them we needed to get her packed up and ready to go to the ER they all jumped in to help. The patient stated that they needed to use the restroom and I had one of my assistants accompany her for that. We then loaded her up and buckled into her mother’s car.”
At what point did methemoglobinemia become the suspected cause?
“When I saw that the oxygen saturation had dropped to 73% and the patient was blue it popped into my head. However, I realized that all of her other readings appeared to be normal and it jumped up higher on my differential diagnosis list.”
Looking back, do you see any earlier “red flags” that were missed or delayed in recognition?
“When the patients lips started to turn blue at the end of the appointment was the biggest red flag that I recall. This is where I beat myself up the most in terms of how I handled the situation.”
How was the diagnosis ultimately confirmed?
“I was told that in the ER several diagnostic tests were done. X-rays, blood work, etc. Given that she just had a procedure done at a dental office they decided to give her methylene blue via IV to see how she would respond. After her O2 saturation started to climb back up it confirmed the diagnosis. They had to give her two rounds of methylene blue in total.”
Of the treatment steps you attempted, what worked/didn’t work?
“I would just like to say, most importantly, if you determine that a patient needs to go to the ER to never attempt to have someone drive them. Please call 911. Looking back, I think placing the patient on 100% O2 bought us some time, this was a step that was also taken when the patient was in the ER and they were running diagnostic tests to try and figure out what was happening. Secondly, when the patient became unconscious and non-responsive while in the car, I believe it was very important to get her out of a car and lay her in a safe place on the ground. Once it was noted that the patient was taking breaths (though very small and hardly noticeable), doing assisted breathing with the ambu bag [Bag Valve Mask-BVM] seemed to help a lot. Make sure to remember the head tilt-and chin lift technique. This is very important. The assisted breathing seemed to help her begin to take deeper breaths. During this stage we continue to try to keep the patient conscious and as alert as possible by talking to her and patting her on the neck and cheek when she would begin to close her eyes a bit. As a side note, if there is family involved in the emergency, I would say to try to include them as little as possible in the life-saving steps. We don't know for sure how people respond to emergencies. The mother in this instance could not figure out how to work a cell phone to call 911. This isn't something that I fault her for at all given how traumatizing this experience was. Thankfully in today’s world everyone has cell phones and one of my assistants was able to make the call and have my hygienist speak with the operator as we supported the patients breathing.”
If you had methylene blue available to you, do you feel you would have administered it?
“The methylene blue needs to be administered via IV which is something I'm not trained with at this point in my career. I would just say that at this point the diagnosis could have been entirely something else in theory. I wouldn't take a chance in giving methylene blue even if I did have it on hand. I think that when a patient starts to show these signs it’s most important to call 911 and get them to the ER. What if it’s not this rare disease but a pulmonary embolism or some other medical emergency?”
How did the patient’s status evolve?
“Both during your care and once EMS or hospital care was involved? > She began taking deeper breaths and would open her eyes for us on command, which was a big improvement. Once EMS arrived, they also hooked her up to a portable capnography machine to evaluate the situation. They understandably were not sure about what was occurring either. Her status at the hospital increased significantly once the methylene blue was administered. She had a headache that persisted for several hours but went away by the next day. She stated that she would get dizzy in the first day or two following her hospital stay.”
How is your patient doing now?
“Patient seems to be 100% back to normal and returned to work without missing any days. She's a champ.”
What do you see now as your biggest mistake or blind spot in managing this case?
“First and foremost, I should've never left the office before the patient once I noticed the slight bluing of the lips. This is a rule I have with all of my other patients. Given that this was a staff member that was going to stay after hours to finish up a few things I decided to leave once I convinced myself it was likely nothing.”
What do you feel was absolutely solid about you/your team's response?
“Given that we just had an in office BLS training a month ago my staff knew exactly where all the emergency equipment was and could anticipate my needs at each step. They were quick and efficient with grabbing what we needed. My team was able to function at the highest stress moments of this emergency. They were able to function despite their close personal relationships with the patient. I'm proud of the technique and skill that was shown by all involved to save a life.”
How was your experience with EMS?
“Did you feel they were supportive or not? They were very supportive. They were as perplexed about the whole situation as we were. When I informed them that I had a feeling it could be methemoglobinemia they looked at me like I had 3 heads which I can’t fault them for.”
If you could go back and change one or more things about your preparation or your response, what would it be?
“CALL 911 quicker than you think you need to. Also, make sure your staff knows that they should call 911 in a perceived emergency even if the doctor has not been informed yet.”
How has this shaped the way you practice dentistry and sedation today?
“After handling an emergency like this it has made my procedures seem much less stressful. However, it taught me to not ignore signs that might seem insignificant. Things like blue lips can be a sign for many things and aren't always an emergency, however, emergencies should be ruled out.”
What advice would you give to colleagues to prevent or recognize methemoglobinemia earlier?
“This is an extremely rare but dangerous condition if not treated quickly. There is a wide variety of things that can present in a similar fashion. With that being said, this was a young healthy patient and many of those other conditions aren't typical in someone such as this. Our [monitoring] equipment showed that the patient’s cardiac rhythms were perfectly fine but that her oxygen saturation was dangerously low. The biggest takeaway would be to not try and treat this yourself and to just call 911. Give as much information to EMS as possible to aid in a differential diagnosis.”
How did this experience affect you personally–in terms of confidence, stress, or your approach to patient safety?
“Overall it boosted my confidence. It showed me not only how I would respond in an emergency situation, but also how my staff would respond as well. I really cannot commend them enough. I'm very grateful for each and every one of them for their help and preparation to handle this situation. As far as a patient safety standpoint is concerned, I'll be much quicker to call 911 when needed. I'd rather the paramedics tell me that a patient doesn't need to go to the hospital than having a patient undergo a life threatening event.”
How has your team responded? Immediately and now afterwards?
“My team was understandably shaken up initially. It's not easy to see anyone appear lifeless in an emergency situation, but for them it was someone that they work with and are friends with which made it worse for them. Certain team members were affected more than others, which was hard to see. But now that it has been a couple of weeks all of them seem to be doing much better. I've spoken with them quite a bit about the event to help them unpack what happened, and to also give them a lot of praise. I've encouraged certain members to reach out to a therapist if they feel that they need it. The last thing I would want is for any of them to get PTSD from this.”
What systems or training have you changed in your practice since then (monitoring, drug selection, team drills)?
“We have really emphasized the fact that if they (our team) feel like a patient is having an emergency to call 911 even if a doctor isn't present or hasn’t been notified. We have really driven home the point that calling emergency services early is paramount.”
Do you feel that methemoglobinemia is underrecognized in dental and surgical training, and what would you like to see emphasized more?
“I think its certainly something that is very rare and its understandably forgotten once you leave dental school. I never thought I would see methemoglobinemia at any point in my career. So I'm not sure that its underrecognized, but its definitely something we need to be aware of. In the end, it's likely that when I mentioned this condition to the paramedics that it was then put on their radar. Who knows, maybe this played a role in saving her life.”
If you could leave our readers with one “non-negotiable” pearl of wisdom from this experience, what would it be?
“If you think a patient is having a possible emergency do not try and have someone drive them to the ER even if the patient is alert and cognitively "normal". This could be fatal. Just call 911.”
The Science Behind the Blue
Methemoglobinemia occurs when hemoglobin is oxidized to methemoglobin, which can’t carry oxygen effectively. Instead of delivering oxygen, it hangs on to it—like a bus driver refusing to let passengers off at the stop.
Classic signs: cyanosis (blue lips/skin that doesn’t improve with O2), headache, fatigue, confusion, tachycardia, and in severe cases, loss of consciousness. Some literature states that even upon administering high flow O2, patients will not exceed 83% SpO2.
Prevalence: An estimated 1–2% of the general population carries genetic variants that predispose them, but drug-induced cases are far more common.
Common triggers in dentistry/medicine include:
- Topical anesthetics: benzocaine (the biggest offender), prilocaine
- Injectable anesthetics: articaine, lidocaine (rare)
- Other drugs: dapsone, nitrates/nitrites, sulfonamides
Safer alternatives: For at-risk patients, consider avoiding benzocaine entirely, and opt for lidocaine or mepivacaine in limited doses.
The Treatment Protocol
Once recognized, treatment is straightforward but urgent. According to Praxis Medical Insights: Practical Summaries of Clinical Guidelines, 2025
- Stop the offending drug.
- Administer 100% oxygen with rescue breaths if needed at one breath per six seconds.
- Confirm diagnosis (via co-oximetry (this is a blood analysis technique that uses multiple wavelengths of light to directly measure different forms of hemoglobin-- oxyhemoglobin, deoxyhemoglobin, carboxyhemoglobin, and methemoglobin), if available—pulse oximetry alone may mislead).
- Methylene blue IV at 1–2 mg/kg over 5 minutes is the universally accepted antidote. May administer an additional 1mg/kg if inadequate response after 30-60 minutes. Do NOT exceed maximum total dose of 7mg/kg due to risk of toxicity.
- Supportive measures: airway management, fluids, monitoring. Odd Fact: In the absence of methylene blue, high-dose ascorbic acid (vitamin C) can sometimes be used—but it’s the “duct tape fix,” not the gold standard.
Takeaways for Dental Teams
- Blue lips aren’t always “just cold.”
- Pulse oximetry may show stubbornly low values despite O2 therapy—red flag.
- Call 911 early. You’ll never regret over-calling, but you’ll always regret under-calling.
- Stock knowledge over methylene blue if you don’t have the skill base to administer it.
Final Word
This case is a reminder that rare doesn’t mean impossible. Dr. Flint’s calm leadership, rapid teamwork, and willingness to reflect openly provide a blueprint for all of us. Emergencies don’t just test patients—they test us, our systems, and our humility. Thank you for sharing Dr. Flint. May we all be a little better prepared now.
Travis V. Coulter, DDS
Clinical Director, Xchart.com travis@Xchart.com
Images
Important: The patient depicted in these images has provided informed written consent on a HIPAA-compliant authorization form, expressly granting permission for the use, reproduction, and public distribution of these photographs — including publication on Xchart’s public blog, as well as in newsletters, print, and digital media — for educational, promotional, and professional purposes. The patient understands that once published, these images may be accessible to the general public and waives any right to royalties or other compensation related to their use.
Closeup of face:
Being treated by EMS:

Dr. Flint posing with recovering patient:
